Osteochondrosis does not cause pain, but at the same time, pain may occur with osteochondrosis. A strange situation, at first glance. But after reading this article, he will become a real expert not only on this topic, but also on: What is osteochondrosis? What are the reasons? What are the symptoms and signs? How to diagnose osteochondrosis? What effective treatment exists? What is included in the prevention of this disease? And also on many other issues.
What is osteochondrosis?
To understand what osteochondrosis is, it is necessary to delve a little into history. The term was introduced in 1928 by Christian Georg Schmorl. But the curious thing is that Schmorl was a pathologist and, as you will understand, he had no one to ask: "Where does it hurt? "(sorry for the dark humor). During his studies of pathological material, Schmorl discovered previously unknown changes in the junction of bone and cartilage, particularly in the area of the intervertebral discs. Once these changes were described, the only thing left to do was find a name for them. For this, he took the Latin word "bone" / os and the Greek word "cartilage" / chondros and, combining them, he received the term osteochondrosis.
What is osteochondrosis? What exactly did Schmorl call this word? It turns out that this is not any pain and generally not a sensation. With the word osteochondrosis, Schmorl designated the following three changes:
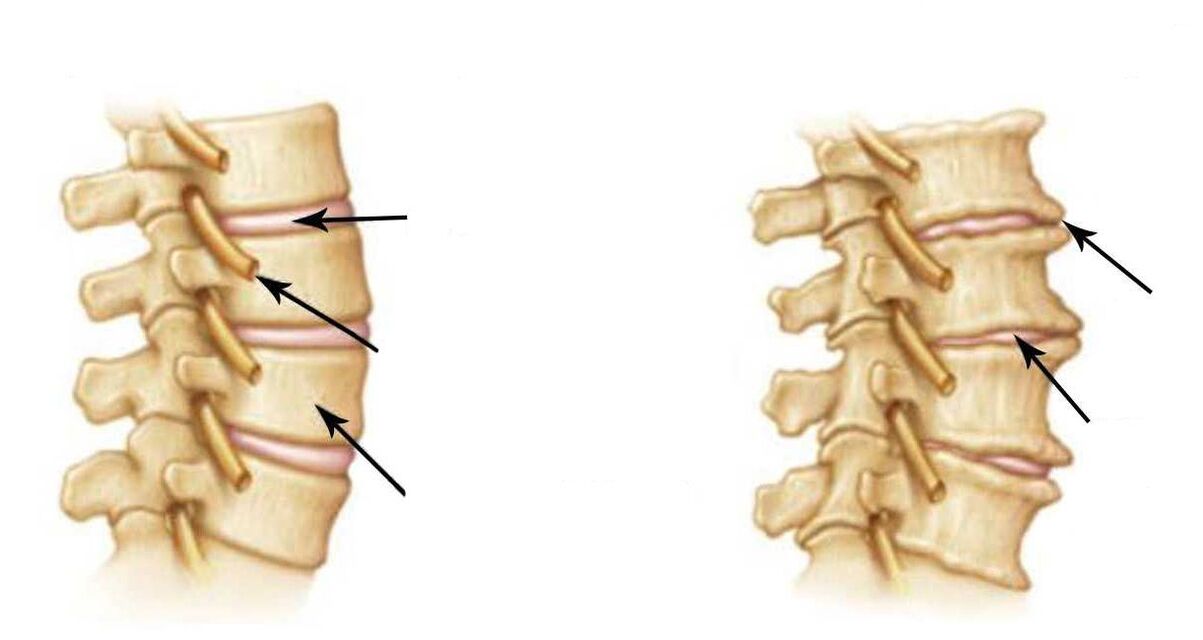
- decreased height of the intervertebral disc;
- subchondral sclerosis;
- Marginal bone growths.
Translated into ordinary language, this means that the height of the disc has decreased and the surface of the vertebra adjacent to the disc has become denser and grown in the form of an edge. This is osteochondrosis in its original meaning, given by Christian Georg Schmorl.
Osteochondrosis disease

Once again, let's pay attention to the fact that Schmorl did not describe the disease osteochondrosis, but only tissue changes, and these are different things. The concept of "disease" is much broader; includes complaints, symptoms, laboratory and radiological changes, treatment and prevention methods.
But Schmorl did not write about any of that and in general did not consider osteochondrosis a disease. But why then is it customary to say that osteochondrosis is a disease, to be interested in the causes of its appearance, its signs, symptoms and treatment of osteochondrosis?
But the fact is that Schmorl had followers. So they decided to find out how osteochondrosis manifests itself and what symptoms bother a person. As a result, it was found that osteochondrosis itself does not directly cause pain and other sensations. This is explained by the fact that there are no pain receptors in the vertebrae and discs. And since there are no receptors, there can be no pain. This is easy to understand using the example of hair and nails: there are also no receptors and no pain when they are cut.
The second important discovery was that osteochondrosis is part of a general degenerative process that encompasses all our organs and tissues. Dystrophy is a violation of tissue nutrition at the cellular level, lasts a lifetime and gradually ages our body. That is, osteochondrosis is essentially part of the aging process. But, as you know, details matter. And the detail is that not all degenerative processes are as painless as osteochondrosis. In particular, dystrophic pathology of the muscles surrounding the spine is almost always associated with pain. After all, muscles, unlike vertebrae and discs, have pain receptors. A typical example is myofascial syndrome. It usually occurs in parallel with osteochondrosis and is painful. Now, remember, at the beginning of the article we said that osteochondrosis itself does not cause pain, but is pain possible? So, it is precisely these cases, when a painful pathology is added to painless osteochondrosis, the myofascial syndrome itself, that perfectly explain the meaning of what has been said.

You may be wondering where the answer is to the question why it is customary to say that osteochondrosis is a disease? Well, actually we're already close to it. The fact is that, although osteochondrosis itself is not, in fact, a disease, but rather a starting point in the study of degenerative processes, the word "osteochondrosis" has become so entrenched in our language that, over time , has become a slang name that generalizes all spinal diseases.
Causes of osteochondrosis
The reasons can be divided into external and internal.
Internal (endogenous) causes include, first of all, the degenerative process that we discussed previously. This also includes genetic predisposition, as well as hormonal, mineral, vitamin, protein and other metabolic disorders, as a result of which bone and cartilage tissue does not receive the necessary nutrition. All these are the so-called biological factors, which, of course, can be influenced, but doing so is quite difficult and expensive. Despite this, there are simple and inexpensive methods that allow you to achieve no less convincing results by eliminating only external causes.
External (exogenous) reasons are considered to be a sedentary lifestyle, poor training of the muscles of the spinal corset, microtrauma of the back and spine, insufficient physical activity, the habit of slouching, "sedentary" work, constant stressful situations, the lack of preventive visits. to a chiropractor and much more.
As you can see, external reasons are largely due to our incorrect actions, for example, low physical activity, or our inaction and neglect of our health, for example, ignoring prevention.
Agree, external causes are much easier to eliminate than internal ones. Of course, there are patients who cannot do without pharmacological treatment for internal reasons, but they are few. In most cases, it is enough to eliminate the external causes of osteochondrosis to obtain convincing results at a lower cost. This will require some self-discipline, basic physical activity, and regular visits to a chiropractor.
Symptoms and signs of osteochondrosis
Symptoms and signs are generally divided into those that develop within the spine itself and those that are extravertebral in nature.
What do you think are the symptoms of osteochondrosis that cause the most problems? In fact, a lot depends not only on the symptoms themselves, but also on other factors: age, weight, presence of concomitant diseases in the patient, etc.
But let's return to the symptoms of vertebral osteochondrosis: as we said, they are vertebral, they are also called vertebral and extravertebral - extravertebral. Extravertebral symptoms, in turn, are also divided into two groups: reflex and radicular symptoms of osteochondrosis.
For simplicity, this classification of back symptoms is best represented as follows:
- Vertebrates/vertebrals
- Extravertebral/extravertebral: radicular symptoms and reflex symptoms
Spinal symptoms of osteochondrosis include curvature of the spine (not to be confused with scoliosis), local pain, muscle tension, and reduced mobility.
Radicular symptoms occur due to effects on the nerves exiting the spine. This is manifested by decreased reflexes, muscle weakness, altered sensitivity and radicular pain.
And here it is necessary to explain that all our vertebrae, discs and "roots" have a certain designation. Therefore, we can talk about radicular symptoms only when all these symptoms and signs clearly indicate a specific "root", and not when any "bulldozer" pain is called radicular.
Very rare, but dangerous signs and symptoms of osteochondrosis are paresis, paralysis and disruption of the pelvic organs. They indicate the development of a spinal stroke. This is a serious complication of osteochondrosis, in which the root arteries are affected.

Reflex symptoms depend mainly on which part of the spine is affected. According to statistics, the cervical spine is the most affected.
The essence of cervical osteochondrosis is a large number of reflex symptoms. Pain in the neck, neck and neck area. Cracking of the vertebrae, muscle tension and difficulty moving. Headache. Dizziness. Intracranial pressure. Morning stiffness. Numbness, tingling, goosebumps and weakness in the arms. Pain in the shoulders and under the shoulder blade. Burning between the shoulder blades and in the area of the heart (reminiscent of angina). Numbness of the hands or fingers. "Lump" in the area of the seventh cervical vertebra. Temporary darkening or "floaters" in the eyes. Noise or ringing in the ears. Nausea, even vomiting. Sudden increases in pressure. State prior to fainting. A lump in the throat with osteochondrosis, weakening of the voice, hoarseness, a feeling of shortness of breath, problems swallowing and sore throat with osteochondrosis - all these are quite common reflex symptoms. There may also be sleep disturbances, frequent insomnia and a feeling of tiredness in the morning. General weakness. Irritability. Rapid fatigue.
As you can see, the symptoms and signs of osteochondrosis disease are very diverse. This is especially true in the case of reflex symptoms.
Diagnosis of osteochondrosis.
Diagnosis is the key to adequate treatment. Modern hardware diagnostic methods make it possible to accurately confirm this diagnosis. As you know, MRI and CT scan are considered the most accurate examinations. But, as before, the main factor in making a diagnosis remains the clinical diagnosis. In this case, an experienced doctor compares data from at least three sources: the patient's complaints, the results of MRI, and the symptoms identified during the examination.
This diagnostic approach allows you to establish an accurate diagnosis and develop an individual effective treatment program.
Effective treatment of osteochondrosis.
Effective treatment of osteochondrosis is possible only with strict adherence to a scientific approach. This means that correct prioritization is necessary, first of all, when choosing the main and auxiliary types of treatment for vertebral osteochondrosis.
What do you think is the most important treatment? You don't have to be a doctor to answer this question. You can just follow the logic. Osteochondrosis is a pathology of the musculoskeletal system. This system is biomechanical in nature. The key word is "mechanics. "Consequently, mechanical disorders require the same (mechanical) treatment methods. Therefore, the main type of treatment for osteochondrosis is manual therapy. It is ideal for restoring the biomechanics of the musculoskeletal system. And auxiliary methods include medication, physiotherapy, massage, physiotherapy, etc. And it is also important to know that among all types of manual treatment, the safest is gentle manual therapy. It is superior to conventional manual therapy due to its effectiveness, gentleness and safety. To understand what the treatment of osteochondrosis by a chiropractor entails, it is necessary to know that the intervertebral discs are the only part of the body that does not have blood vessels and is nourished thanks to the proper functioning of the spinal muscles. Failure in the functioning of these muscles immediately impairs the nutrition of the discs. And as we said at the beginning of the article, malnutrition is the degenerative process of which osteochondrosis is a part.
Effective treatment with gentle manual therapy is fundamentally different from conventional manual therapy. This is not at all a "spinal realignment" as some people think, it is something completely different. Gentle manual therapy is a complete system of special methods of influence that eliminate muscle spasms and tension. Return muscles to their normal physiology and improve nutrition of the discs.
Observation by a doctor includes three stages:
- Consultation. The doctor finds out what symptoms worry the patient, clarifies the medical history, studies the patient's medical documentation, analyzes images and determines the nature of the disease.
- Diagnosis. Conducts a comprehensive examination and clinical examination of the patient: visual and myofascial diagnosis; palpation of tense muscles and painful vertebrae; neurological reflex tests and muscle tests.
- Treatment plan. Based on the history of the current illness, examination data, as well as the results of the patient's clinical examination, the doctor makes a diagnosis and selects treatment options. The doctor informs the patient in detail about the essence of the disease and the principles of treatment, and answers all of the patient's questions.
Prevention of osteochondrosis
Prevention is necessary to avoid relapses. To do this, you need to create comfortable conditions for work and rest. Maintain physical activity. Avoid overwork. Monitor adequate nutrition and weight. But the main thing is not to neglect your health.
Remember, prevention is, first of all, medical supervision and timely correction of the musculoskeletal system. Try to visit a chiropractor at least once every three to six months. This will reduce risk factors and eliminate any violations in a timely manner. Advanced osteochondrosis leads to complications: bulges and herniated discs. Do not forget this. Take care of yourself!


















